Key Takeaways
A PCOS diet is the best foundational treatment for managing PCOS. But dietary supplements can help a lot too. The challenge here is sorting the wheat from the chaff. The 15 supplements described below are the most well-supported by solid scientific evidence.
1. Myo-inositol
Of all the many PCOS supplements, inositol is one of the best. Ovasitol by Theralogix is the leading brand for the treatment of PCOS. Inositol supplements improve insulin sensitivity and blood sugar regulation [1, 2]. This has a cascading effect on hormone balance that can alleviate a wide range of common PCOS symptoms.
Myo-inositol can improve fertility and reduce the risk of gestational diabetes [3-7]. It can also help some women reduce acne and unwanted facial hair growth [8, 9]. Inositol supplements appear to be better than metformin for menstrual regularity and metabolic disorders [10, 11]. It’s also much better tolerated as side effects are minimal.
Despite popular belief, myo-inositol isn’t one of the best supplements for PCOS weight loss. It’s great for your health. But weight loss benefits (if any) are insignificantly small [12-14].
Learn more about inositol supplements for PCOS here.
2. B-Vitamins
There are a lot of different B vitamins. All of which serve an important role in health and fertility. But B12 and B9 (folate/folic acid) are the most salient for polycystic ovarian syndrome. These B vitamins play a key role in regulating the amino acid, homocysteine. Homocysteine is elevated in PCOS. This leads to an increased risk for cardiovascular and reproductive problems [15-17]. B vitamin supplementation can lower these risks [18].
The most important time to consider B vitamin supplements is before pregnancy. For women with PCOS, it’s important to avoid folic acid. PCOS is associated with MTHFR gene mutations [19, 20]. If you have this mutation, then taking folic acid during pregnancy can affect your child’s lung function [21]. What you want instead, is the active form of folate (methyl folate) [22].
TheraNatal® Core Preconception Vitamins is one of the best prenatal supplements for PCOS. This product contains methyl folate rather than folic acid.
Experts also recommend testing and supplementing B vitamins whenever metformin is used. Metformin is well-known to deplete nutrients.
3. Vitamin D
Vitamin D supplementation has been studied extensively in polycystic ovary syndrome patients. The well-established benefits include:
- Improved hormone levels, inflammation, and oxidative stress [23].
- Reduced insulin resistance and hyperandrogenism [24-26].
- Improved lipid metabolism and triglycerides [24, 26-28].
There is strong evidence that these benefits improve fertility and menstrual cycle regulation [29-31]. Fertility treatment outcomes are also better with adequate vitamin D levels [32-34].
Unfortunately, approximately 67 – 85% of women with PCOS have vitamin D deficiency [35]. These risks are highest in people with darker skin tones that live in northern climates [36-40].
Vitamin D is one of the most important of all PCOS vitamin supplements. Learn more about dosing and brands here.
4. Magnesium
More than half of Americans have inadequate dietary intake of magnesium [41]. Rates are even higher among PCOS women [42]. That’s because many of the risk factors for insufficient magnesium are common in PCOS. This includes being overweight, having insulin resistance, and taking medications [43-49].
Taking magnesium supplements has a significant effect on PCOS hormone imbalances [50]. On its own, it can help with weight loss, high blood pressure, and PCOS period pain [50-53]. When combined with other PCOS vitamins and supplements, magnesium can also help with glucose metabolism, hirsutism, anxiety, and quality of life [54-59].
Learn more about magnesium supplements for PCOS here. This article includes tips on blood testing, safety info’, and recommended products.
5. Zinc
There’s a good reason that you’ll find zinc on most lists of the best supplements for PCOS.
Insufficient zinc levels are a common problem for PCOS patients. This contributes to the hormone imbalances that cause PCOS symptoms [60, 61].
This is a relatively easy problem to fix. Zinc supplementation in PCOS patients can improve hormonal imbalances. This reduces the risks of insulin resistance and cardiovascular disease [61]. At least one clinical trial has also shown the value of zinc supplements for PCOS hair loss and hirsutism [62].
Zinc is best taken as part of a multivitamin product like Women’s Multi 50+ by Thorne Research. This product includes 15 mg of zinc as TRAACS® Zinc Bisglycinate. This is a bioavailable form of zinc. It also includes a lot of the other PCOS vitamin supplements included in this article. Most importantly, products like Women’s Multi 50+ exclude copper and iron. This is important because PCOS women tend to have high levels of these nutrients [63].
6. Chromium
Chromium picolinate has been shown to improve insulin resistance and metabolic health in women with PCOS [64, 65]. Trials using 200 μg/day have observed reduced rates of hirsutism and acne [66].
Like all PCOS supplements, it’s important to consider individual differences when using chromium. In most cases, the size of the effect is likely to be small.
7. Fish Oil
Fish oil and the omega-3 fatty acids they contain are widely understood to be good for cardiovascular health. Omega-3 fats reduce inflammation which is one of the underlying drivers of all PCOS symptoms. This suggests that there may be widespread benefits from taking omega-3 supplements for PCOS. But these have not been sufficiently demonstrated in clinical trials. In PCOS patients, decreasing cholesterol levels is the most well-proven benefit [67].
Fish oil supplements have also been used for reducing PCOS period pain. Studies suggest that 1,000 mg/day of fish oil is better than taking Advil (Neurofen) [68, 69].
One of the best fish oil supplements for PCOS is Nordic Naturals Ultimate Omega. This product was used in a high-quality trial that demonstrated the health benefits of omega-3 supplements for PCOS women [70].
8. CoQ10
Coenzyme Q10 (CoQ10) is an antioxidant that has anti-inflammatory properties. This means it can combat chronic inflammation, one of the underlying mechanisms that drive all PCOS symptoms [71-74].
CoQ10 has been well-studied as a PCOS treatment. A recent systematic review and meta-analysis found the following benefits [75]:
- Improvements in insulin resistance, fasting insulin, and fasting plasma glucose.
- Better sex hormone balance.
- Improved triglycerides and cholesterol levels.
- CoQ10 is not associated with adverse effects. It’s a safe therapy.
Because CoQ10 is only soluble in fat, many formulations are not well absorbed in the gut. Proprietary formulations like VESIsorb increase the absorption of CoQ10 by more than 600% compared with standard oil-based CoQ10 [76]. It’s also many times more bioavailable than solubilized formulations.
NeoQ₁₀ by Theralogix uses the patented VESIsorb technology. This product can be purchased online here.
9. Curcumin
Curcumin is a naturally occurring compound with potent anti-inflammatory and antioxidant effects. This well-tolerated plant-derived medicine has been widely studied for a range of conditions [77]. In women with PCOS, curcumin can improve cardiovascular health and help with weight loss [78].
Curcumin is an excellent alternative medication for PCOS pain. For example, a two-gram dose of the proprietary formulation, Meriva, can produce comparable pain relief to two Tylenol (Panadol) extra-strength tablets [79].
It’s important when buying curcumin supplements to look for advanced delivery systems (like Meriva) that increase bioavailability. It’s unlikely that cheaper formulations of turmeric root extract will achieve the same therapeutic effect [80-82].
10. Melatonin
Out of all the many PCOS supplements, melatonin may be one of the most underrated. Like vitamin D, melatonin has massive impacts on health [83].
Women with PCOS have lower melatonin concentrations. This doesn’t just impact sleep. Ovarian function is also affected [84]. This drives a lot of the hormone imbalances common in PCOS. Yet studies show that supplementation can reduce these effects [85-87].
Melatonin supplementation makes sense if you’re trying to conceive or get your period back. It also makes sense if you have difficulty losing weight or you want to reduce excessive hair growth and other signs of hirsutism [88, 89].
11. NAC
The research on N-acetylcysteine (NAC) for PCOS has produced mixed results, largely as a result of biases in study design. This has presented challenges in determining its appropriate use and clinical value.
Based on the most recent reviews of the evidence though, NAC appears to be one of the better supplements to treat PCOS. In PCOS patients, NAC can reduce testosterone levels and increase follicle-stimulating hormone levels [90]. One analysis found that it was better than metformin for weight management and lowering total testosterone [91]. Others have shown that it’s superior for improving fasting blood sugar and fasting insulin levels [92].
These benefits translate into real-life outcomes. For example, NAC improves pregnancy rates. It may be particularly beneficial when combined with clomid or letrozole [93, 94].
12. Berberine
Berberine is one of the few herbal supplements with pharmaceutical-level effects. This is a great option for insulin-resistant PCOS women that aren’t trying to conceive.
Many clinical trials have shown that berberine is at least as good as metformin for treating insulin resistance in PCOS patients [95-97]. It’s also good for blood pressure, weight loss, and other markers of metabolic health [97-101].
Berberine improves hormone balance and can boost fertility [97, 101]. Many people prefer it to metformin because it has fewer side effects. Berberine is a relatively safe supplement, but it’s important to check drug interactions before use.
Learn more about berberine including dosage, safety, and the best brands here.
13. Resveratrol
Resveratrol is a natural antioxidant found in grapes, nuts, and berries. Its use as a PCOS supplement mostly centers around its anti-inflammatory properties and its effect on the ovaries [102-104]. Studies have shown that resveratrol can improve menstrual regularity in PCOS women [105].
Care is needed when supplementing with resveratrol. It shouldn’t be used during the luteal phase of your cycle and may not be safe during pregnancy [106].
14. Cinnamon
Cinnamon is an ancient traditional medicine. It’s also one of the best herbs for PCOS. Several reviews have shown that cinnamon can improve metabolic parameters in PCOS patients [107-109]. These include fasting blood sugar, fasting insulin, cholesterol, and triglyceride levels.
Cinnamon is generally considered a safe supplement. But higher doses of 1.5 g/day are needed for the best clinical outcomes [109].
15. Probiotics and Prebiotics
Poor gut health may be one of the underlying causes of PCOS. Dysbiosis of the gut microbiome can account for all three components of a PCOS diagnosis [110, 111]. It can also cause insulin resistance in women with PCOS [112]. So, the growing popularity of prebiotic and probiotic supplements for PCOS makes good sense.
Several meta-analyses show the benefits of probiotics and prebiotics for the treatment of PCOS [113, 114]. They appear to improve many hormonal and inflammatory markers. They can help with insulin sensitivity, weight gain, and cardiovascular health. They can also lower testosterone levels and relieve hirsutism.
The greatest challenge with using prebiotic and probiotic supplements for PCOS is picking the right type. Many over-the-counter products may not be worth the cost.
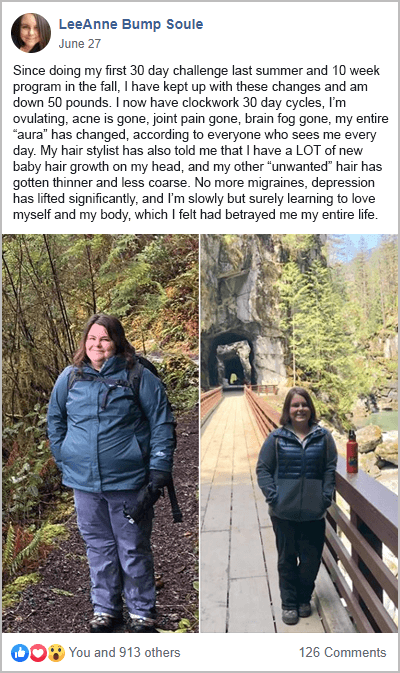
But following a PCOS diet is. Adding more prebiotic and probiotic foods into your diet can help improve gut health. Cutting out the foods to avoid with PCOS, makes a big difference too. The benefits of these steps have been well-demonstrated by participants from my free 30-Day PCOS Diet Challenge.
The Bottom Line
Nutritional supplements are a valuable intervention for women with polycystic ovary syndrome. In some cases, dietary supplements can be as effective as pharmaceutical drugs. But often with fewer side effects.
The 15 compounds described above provide a good short-list for consideration. A naturopathic or functional medicine doctor can help you determine which of these supplements are best for you.
Irrespective of your drug or supplement protocol, a PCOS-friendly diet will help you achieve the best health outcomes. To get started today, join my free 30-Day PCOS Diet Challenge or download this free 3-Day Meal Plan.
FAQ
What are the best supplements for PCOS weight loss? The most effective PCOS weight loss supplements are those that help improve insulin sensitivity. These include inositol, vitamin D, magnesium, zinc, chromium, berberine, cinnamon, and CoQ10. Curcumin, melatonin, and probiotics may also be helpful. It’s important to keep in mind that the strength of the effect is very small for all of these PCOS weight loss supplements. Even modest dietary changes are likely to overshadow any benefits. Learn more about how to lose weight with PCOS here.
What are the best PCOS fertility supplements? Myo-inositol and products like Ovasitol are the most well-proven PCOS fertility supplements. TheraNatal® Core Preconception Vitamins, are another obvious choice. For women undergoing IVF, supplementation with NeoQ₁₀ is recommended [115]. Many of the other supplements listed above may also help you conceive.
What are the best supplements for PCOS hair loss? The treatment of hair loss requires supplements that lower testosterone in PCOS. NAC may be one of the best options. But myo-inositol, B vitamins, vitamin D, magnesium, zinc, chromium, CoQ10, and melatonin may also be helpful.
What are the best PCOS acne supplements? Like hirsutism and hair loss, PCOS acne supplements need to reduce androgen hormones like testosterone. The most well-proven PCOS acne supplements include myo-inositol, zinc, and vitamin B3 (niacin). Some probiotics may also be helpful [116]. Learn more about the best ways to treat PCOS acne here.
What about all the other supplements I read about online? The list above is not exhaustive. But it includes products that have been the most well-proven in PCOS patients. That said, other supplements may be useful as part of a holistic PCOS treatment plan. Products like selenium, carnitine, CBD oil, licorice root, maca root, saw palmetto, vitex, and many others may be helpful too. A naturopathic or functional medicine doctor can help you determine what’s best for you.
Author
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.
References
1Kamenov, Z. and A. Gateva, Inositols in PCOS. Molecules, 2020. 25(23).
2Unfer, V., et al., Effects of myo-inositol in women with PCOS: a systematic review of randomized controlled trials. Gynecol Endocrinol, 2012. 28(7): p. 509-15.
3Artini, P.G., et al., Endocrine and clinical effects of myo-inositol administration in polycystic ovary syndrome. A randomized study. Gynecol Endocrinol, 2013. 29(4): p. 375-9.
4Raffone, E., P. Rizzo, and V. Benedetto, Insulin sensitiser agents alone and in co-treatment with r-FSH for ovulation induction in PCOS women. Gynecol Endocrinol, 2010. 26(4): p. 275-80.
5Emekçi Özay, Ö., et al., Myo-inositol administration positively effects ovulation induction and intrauterine insemination in patients with polycystic ovary syndrome: a prospective, controlled, randomized trial. Gynecol Endocrinol, 2017. 33(7): p. 524-528.
6Sobota-Grzeszyk, A., M. Kuźmicki, and J. Szamatowicz, Myoinositol in the Prevention of Gestational Diabetes Mellitus: Is It Sensible? J Diabetes Res, 2019. 2019: p. 3915253.
7D’Anna, R., et al., Myo-Inositol for the Prevention of Gestational Diabetes Mellitus. A Brief Review. J Nutr Sci Vitaminol (Tokyo), 2019. 65(Supplement): p. S59-s61.
8Minozzi, M., G. D’Andrea, and V. Unfer, Treatment of hirsutism with myo-inositol: a prospective clinical study. Reprod Biomed Online, 2008. 17(4): p. 579-82.
9Zacchè, M.M., et al., Efficacy of myo-inositol in the treatment of cutaneous disorders in young women with polycystic ovary syndrome. Gynecol Endocrinol, 2009. 25(8): p. 508-13.
10Zhao, H., et al., Comparative efficacy of oral insulin sensitizers metformin, thiazolidinediones, inositol, and berberine in improving endocrine and metabolic profiles in women with PCOS: a network meta-analysis. Reprod Health, 2021. 18(1): p. 171.
11Facchinetti, F., et al., Short-term effects of metformin and myo-inositol in women with polycystic ovarian syndrome (PCOS): a meta-analysis of randomized clinical trials. Gynecol Endocrinol, 2019. 35(3): p. 198-206.
12Gerli, S., et al., Randomized, double blind placebo-controlled trial: effects of myo-inositol on ovarian function and metabolic factors in women with PCOS. Eur Rev Med Pharmacol Sci, 2007. 11(5): p. 347-54.
13Le Donne, M., et al., Effects of three treatment modalities (diet, myoinositol or myoinositol associated with D-chiro-inositol) on clinical and body composition outcomes in women with polycystic ovary syndrome. Eur Rev Med Pharmacol Sci, 2019. 23(5): p. 2293-2301.
14Nordio, M. and E. Proietti, The combined therapy with myo-inositol and D-chiro-inositol reduces the risk of metabolic disease in PCOS overweight patients compared to myo-inositol supplementation alone. Eur Rev Med Pharmacol Sci, 2012. 16(5): p. 575-81.
15Badawy, A., et al., Plasma homocysteine and polycystic ovary syndrome: the missed link. Eur J Obstet Gynecol Reprod Biol, 2007. 131(1): p. 68-72.
16Loverro, G., et al., The plasma homocysteine levels are increased in polycystic ovary syndrome. Gynecol Obstet Invest, 2002. 53(3): p. 157-62.
17Yarali, H., et al., Diastolic dysfunction and increased serum homocysteine concentrations may contribute to increased cardiovascular risk in patients with polycystic ovary syndrome. Fertil Steril, 2001. 76(3): p. 511-6.
18Thornburgh, S. and A.J. Gaskins, B vitamins, polycystic ovary syndrome, and fertility. Curr Opin Endocrinol Diabetes Obes, 2022. 29(6): p. 554-559.
19Li, Y., et al., Significant association between methylenetetrahydrofolate reductase gene C677T polymorphism with polycystic ovary syndrome risk: A meta-analysis update. Medicine (Baltimore), 2020. 99(4): p. e18720.
20Zhu, X.Y., et al., Association of methylenetetrahydrofolate reductase C677T and A1298C polymorphisms with genetic susceptibility to polycystic ovary syndrome: A PRISMA-compliant meta-analysis. Gene, 2019. 719.
21den Dekker, H.T., et al., Maternal folic acid use during pregnancy, methylenetetrahydrofolate reductase gene polymorphism, andchild’s lung function and asthma. Clinical and Experimental Allergy, 2018. 48(2): p. 175-185.
22Serapinas, D., et al., The importance of folate, vitamins B6 and B12 for the lowering of homocysteine concentrations for patients with recurrent pregnancy loss and MTHFR mutations. Reprod Toxicol, 2017. 72: p. 159-163.
23Zhao, J.F., B.X. Li, and Q. Zhang, Vitamin D improves levels of hormonal, oxidative stress and inflammatory parameters in polycystic ovary syndrome: a meta-analysis study. Ann Palliat Med, 2021. 10(1): p. 169-183.
24Miao, C.Y., et al., Effect of vitamin D supplementation on polycystic ovary syndrome: A meta-analysis. Exp Ther Med, 2020. 19(4): p. 2641-2649.
25Łagowska, K., J. Bajerska, and M. Jamka, The Role of Vitamin D Oral Supplementation in Insulin Resistance in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients, 2018. 10(11).
26Wang, L., et al., Effects of vitamin D supplementation on metabolic parameters of women with polycystic ovary syndrome: a meta-analysis of randomized controlled trials. Gynecol Endocrinol, 2021. 37(5): p. 446-455.
27Luo, J., T. Li, and J. Yuan, Effectiveness of vitamin D supplementation on lipid profile in polycystic ovary syndrome women: a meta-analysis of randomized controlled trials. Ann Palliat Med, 2021. 10(1): p. 114-129.
28Gao, H., et al., The Effect of Vitamin D Supplementation on Blood Lipids in Patients with Polycystic Ovary Syndrome: A Meta-Analysis of Randomized Controlled Trials. Int J Endocrinol, 2021. 2021: p. 8849688.
29Fang, F., et al., Effect of vitamin D supplementation on polycystic ovary syndrome: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract, 2017. 26: p. 53-60.
30Shojaei-Zarghani, S. and M. Rafraf, Resveratrol and Markers of Polycystic Ovary Syndrome: a Systematic Review of Animal and Clinical Studies. Reprod Sci, 2021.
31Moridi, I., et al., The Association between Vitamin D and Anti-Müllerian Hormone: A Systematic Review and Meta-Analysis. Nutrients, 2020. 12(6).
32Chu, J., et al., Vitamin D and assisted reproductive treatment outcome: a systematic review and meta-analysis. Hum Reprod, 2018. 33(1): p. 65-80.
33Zhang, H., et al., Meta-analysis of the effect of the maternal vitamin D level on the risk of spontaneous pregnancy loss. Int J Gynaecol Obstet, 2017. 138(3): p. 242-249.
34Pilz, S., et al., The Role of Vitamin D in Fertility and during Pregnancy and Lactation: A Review of Clinical Data. Int J Environ Res Public Health, 2018. 15(10).
35Thomson, R.L., S. Spedding, and J.D. Buckley, Vitamin D in the aetiology and management of polycystic ovary syndrome. Clin Endocrinol (Oxf), 2012. 77(3): p. 343-50.
36Munns, C.F., et al., Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. J Clin Endocrinol Metab, 2016. 101(2): p. 394-415.
37van Schoor, N. and P. Lips, Global Overview of Vitamin D Status. Endocrinol Metab Clin North Am, 2017. 46(4): p. 845-870.
38Cashman, K.D., et al., Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr, 2016. 103(4): p. 1033-44.
39Palacios, C. and L. Gonzalez, Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol, 2014. 144 Pt A: p. 138-45.
40Forrest, K.Y. and W.L. Stuhldreher, Prevalence and correlates of vitamin D deficiency in US adults. Nutr Res, 2011. 31(1): p. 48-54.
41Workinger, J.L., R.P. Doyle, and J. Bortz, Challenges in the Diagnosis of Magnesium Status. Nutrients, 2018. 10(9).
42Kazemi, M., et al., Comparison of dietary and physical activity behaviors in women with and without polycystic ovary syndrome: a systematic review and meta-analysis of 39471 women. Hum Reprod Update, 2022. 28(6): p. 910-955.
43Babapour, M., et al., Associations Between Serum Magnesium Concentrations and Polycystic Ovary Syndrome Status: a Systematic Review and Meta-analysis. Biol Trace Elem Res, 2021. 199(4): p. 1297-1305.
44Chakraborty, P., et al., Altered trace mineral milieu might play an aetiological role in the pathogenesis of polycystic ovary syndrome. Biol Trace Elem Res, 2013. 152(1): p. 9-15.
45Hamilton, K.P., et al., Insulin Resistance and Serum Magnesium Concentrations among Women with Polycystic Ovary Syndrome. Curr Dev Nutr, 2019. 3(11): p. nzz108.
46Sharifi, F., et al., Serum magnesium concentrations in polycystic ovary syndrome and its association with insulin resistance. Gynecol Endocrinol, 2012. 28(1): p. 7-11.
47Xu, L.H. and N.M. Maalouf, Effect of acute hyperinsulinemia on magnesium homeostasis in humans. Diabetes Metab Res Rev, 2017. 33(2).
48Wakeman, M. and D.T. Archer, Metformin and Micronutrient Status in Type 2 Diabetes: Does Polypharmacy Involving Acid-Suppressing Medications Affect Vitamin B12 Levels? Diabetes Metab Syndr Obes, 2020. 13: p. 2093-2108.
49Palmery, M., et al., Oral contraceptives and changes in nutritional requirements. Eur Rev Med Pharmacol Sci, 2013. 17(13): p. 1804-13.
50Farsinejad-Marj, M., et al., Clinical and Metabolic Responses to Magnesium Supplementation in Women with Polycystic Ovary Syndrome. Biol Trace Elem Res, 2020. 196(2): p. 349-358.
51Parazzini, F., M. Di Martino, and P. Pellegrino, Magnesium in the gynecological practice: a literature review. Magnes Res, 2017. 30(1): p. 1-7.
52Asbaghi, O., et al., The Effects of Magnesium Supplementation on Blood Pressure and Obesity Measure Among Type 2 Diabetes Patient: a Systematic Review and Meta-analysis of Randomized Controlled Trials. Biol Trace Elem Res, 2021. 199(2): p. 413-424.
53Zhang, X., et al., Effects of Magnesium Supplementation on Blood Pressure: A Meta-Analysis of Randomized Double-Blind Placebo-Controlled Trials. Hypertension, 2016. 68(2): p. 324-33.
54Boyle, N.B., C. Lawton, and L. Dye, The Effects of Magnesium Supplementation on Subjective Anxiety and Stress-A Systematic Review. Nutrients, 2017. 9(5).
55Boyle, N.B., C.L. Lawton, and L. Dye, The effects of magnesium supplementation on subjective anxiety. Magnes Res, 2016. 29(3): p. 120-125.
56Jaripur, M., et al., The effects of magnesium supplementation on abnormal uterine bleeding, alopecia, quality of life, and acne in women with polycystic ovary syndrome: a randomized clinical trial. Reprod Biol Endocrinol, 2022. 20(1): p. 110.
57Shokrpour, M. and Z. Asemi, The Effects of Magnesium and Vitamin E Co-Supplementation on Hormonal Status and Biomarkers of Inflammation and Oxidative Stress in Women with Polycystic Ovary Syndrome. Biol Trace Elem Res, 2019. 191(1): p. 54-60.
58Li, R., et al., The effect of magnesium alone or its combination with other supplements on the markers of inflammation, OS and metabolism in women with polycystic ovarian syndrome (PCOS): A systematic review. Front Endocrinol (Lausanne), 2022. 13: p. 974042.
59Jamilian, M., N.K. Sabzevar, and Z. Asemi, The Effect of Magnesium and Vitamin E Co-Supplementation on Glycemic Control and Markers of Cardio-Metabolic Risk in Women with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Horm Metab Res, 2019. 51(2): p. 100-105.
60Guler, I., et al., Zinc and homocysteine levels in polycystic ovarian syndrome patients with insulin resistance. Biol Trace Elem Res, 2014. 158(3): p. 297-304.
61Nasiadek, M., et al., The Role of Zinc in Selected Female Reproductive System Disorders. Nutrients, 2020. 12(8).
62Jamilian, M., et al., Effects of Zinc Supplementation on Endocrine Outcomes in Women with Polycystic Ovary Syndrome: a Randomized, Double-Blind, Placebo-Controlled Trial. Biol Trace Elem Res, 2016. 170(2): p. 271-8.
63Yin, J., et al., Serum Trace Elements in Patients With Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne), 2020. 11: p. 572384.
64Fazelian, S., et al., Chromium supplementation and polycystic ovary syndrome: A systematic review and meta-analysis. J Trace Elem Med Biol, 2017. 42: p. 92-96.
65Heshmati, J., et al., The Effects of Supplementation with Chromium on Insulin Resistance Indices in Women with Polycystic Ovarian Syndrome: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Horm Metab Res, 2018. 50(3): p. 193-200.
66Jamilian, M., et al., The Effects of Chromium Supplementation on Endocrine Profiles, Biomarkers of Inflammation, and Oxidative Stress in Women with Polycystic Ovary Syndrome: a Randomized, Double-Blind, Placebo-Controlled Trial. Biol Trace Elem Res, 2016. 172(1): p. 72-78.
67Arentz, S., et al., Nutritional supplements and herbal medicines for women with polycystic ovary syndrome; a systematic review and meta-analysis. BMC Complement Altern Med, 2017. 17(1): p. 500.
68Zafari, M., F. Behmanesh, and A. Agha Mohammadi, Comparison of the effect of fish oil and ibuprofen on treatment of severe pain in primary dysmenorrhea. Caspian J Intern Med, 2011. 2(3): p. 279-82.
69Hosseinlou, A., et al., The effects of fish oil capsules and vitamin B1 tablets on duration and severity of dysmenorrhea in students of high school in Urmia-Iran. Glob J Health Sci, 2014. 6(7 Spec No): p. 124-9.
70Vargas, M.L., et al., Metabolic and endocrine effects of long-chain versus essential omega-3 polyunsaturated fatty acids in polycystic ovary syndrome. Metabolism, 2011. 60(12): p. 1711-8.
71Ebejer, K. and J. Calleja-Agius, The role of cytokines in polycystic ovarian syndrome. Gynecol Endocrinol, 2013. 29(6): p. 536-40.
72Repaci, A., A. Gambineri, and R. Pasquali, The role of low-grade inflammation in the polycystic ovary syndrome. Mol Cell Endocrinol, 2011. 335(1): p. 30-41.
73Rostamtabar, M., et al., Pathophysiological roles of chronic low-grade inflammation mediators in polycystic ovary syndrome. J Cell Physiol, 2021. 236(2): p. 824-838.
74Rudnicka, E., et al., Chronic Low Grade Inflammation in Pathogenesis of PCOS. Int J Mol Sci, 2021. 22(7).
75Zhang, T., et al., Efficacy and Safety of Coenzyme Q10 Supplementation in the Treatment of Polycystic Ovary Syndrome: a Systematic Review and Meta-analysis. Reprod Sci, 2023. 30(4): p. 1033-1048.
76Liu, Z.X. and C. Artmann, Relative bioavailability comparison of different coenzyme Q10 formulations with a novel delivery system. Altern Ther Health Med, 2009. 15(2): p. 42-6.
77Shah, M., et al., Multiple health benefits of curcumin and its therapeutic potential. Environ Sci Pollut Res Int, 2022. 29(29): p. 43732-43744.
78Shen, W., et al., Therapeutic effect and safety of curcumin in women with PCOS: A systematic review and meta-analysis. Front Endocrinol (Lausanne), 2022. 13: p. 1051111.
79Di Pierro, F., et al., Comparative evaluation of the pain-relieving properties of a lecithinized formulation of curcumin (Meriva(®)), nimesulide, and acetaminophen. J Pain Res, 2013. 6: p. 201-5.
80Sabet, S., et al., Recent advances to improve curcumin oral bioavailability. Trends in Food Science & Technology, 2021. 110: p. 253-266.
81Yixuan, L., et al., Curcumin production and bioavailability: A comprehensive review of curcumin extraction, synthesis, biotransformation and delivery systems. Industrial Crops and Products, 2021. 172: p. 114050.
82Stohs, S.J., et al., Highly Bioavailable Forms of Curcumin and Promising Avenues for Curcumin-Based Research and Application: A Review. Molecules, 2020. 25(6).
83Minich, D.M., et al., Is Melatonin the “Next Vitamin D”?: A Review of Emerging Science, Clinical Uses, Safety, and Dietary Supplements. Nutrients, 2022. 14(19).
84Li, H., M. Liu, and C. Zhang, Women with polycystic ovary syndrome (PCOS) have reduced melatonin concentrations in their follicles and have mild sleep disturbances. BMC Womens Health, 2022. 22(1): p. 79.
85Jamilian, M., et al., Effects of Melatonin Supplementation on Hormonal, Inflammatory, Genetic, and Oxidative Stress Parameters in Women With Polycystic Ovary Syndrome. Front Endocrinol (Lausanne), 2019. 10: p. 273.
86Mojaverrostami, S., et al., The role of melatonin in polycystic ovary syndrome: A review. Int J Reprod Biomed, 2019. 17(12): p. 865-882.
87Xie, F., et al., Melatonin ameliorates ovarian dysfunction by regulating autophagy in PCOS via the PI3K-Akt pathway. Reproduction, 2021. 162(1): p. 73-82.
88Al-Qadhi, H.I. Effect of Melatonin Supplementation on Serum LH Level and BMI in Women with Polycystic Ovarian Syndrome. 2018.
89Mousavi, R., et al., Effects of Melatonin and/or Magnesium Supplementation on Biomarkers of Inflammation and Oxidative Stress in Women with Polycystic Ovary Syndrome: a Randomized, Double-Blind, Placebo-Controlled Trial. Biol Trace Elem Res, 2022. 200(3): p. 1010-1019.
90Shahveghar Asl, Z., K. Parastouei, and E. Eskandari, The effects of N-acetylcysteine on ovulation and sex hormones profile in women with polycystic ovary syndrome: a systematic review and meta-analysis. Br J Nutr, 2023. 130(2): p. 202-210.
91Song, Y., et al., Comparison of the efficacy between NAC and metformin in treating PCOS patients: a meta-analysis. Gynecol Endocrinol, 2020. 36(3): p. 204-210.
92Javanmanesh, F., et al., A comparison between the effects of metformin and N-acetyl cysteine (NAC) on some metabolic and endocrine characteristics of women with polycystic ovary syndrome. Gynecol Endocrinol, 2016. 32(4): p. 285-9.
93Sandhu, J.K., et al., Oxidative Stress in Polycystic Ovarian Syndrome and the Effect of Antioxidant N-Acetylcysteine on Ovulation and Pregnancy Rate. Cureus, 2021. 13(9): p. e17887.
94Thakker, D., et al., N-acetylcysteine for polycystic ovary syndrome: a systematic review and meta-analysis of randomized controlled clinical trials. Obstet Gynecol Int, 2015. 2015: p. 817849.
95Mishra, N., R. Verma, and P. Jadaun, Study on the Effect of Berberine, Myoinositol, and Metformin in Women with Polycystic Ovary Syndrome: A Prospective Randomised Study. Cureus, 2022. 14(1): p. e21781.
96Li, M.F., X.M. Zhou, and X.L. Li, The Effect of Berberine on Polycystic Ovary Syndrome Patients with Insulin Resistance (PCOS-IR): A Meta-Analysis and Systematic Review. Evid Based Complement Alternat Med, 2018. 2018: p. 2532935.
97Xie, L., et al., The Effect of Berberine on Reproduction and Metabolism in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Control Trials. Evid Based Complement Alternat Med, 2019. 2019: p. 7918631.
98Suadoni, M.T. and I. Atherton, Berberine for the treatment of hypertension: A systematic review. Complement Ther Clin Pract, 2021. 42: p. 101287.
99Guo, J., et al., The Effect of Berberine on Metabolic Profiles in Type 2 Diabetic Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Oxid Med Cell Longev, 2021. 2021: p. 2074610.
100Wei, W., et al., A clinical study on the short-term effect of berberine in comparison to metformin on the metabolic characteristics of women with polycystic ovary syndrome. Eur J Endocrinol, 2012. 166(1): p. 99-105.
101An, Y., et al., The use of berberine for women with polycystic ovary syndrome undergoing IVF treatment. Clin Endocrinol (Oxf), 2014. 80(3): p. 425-31.
102Brenjian, S., et al., Resveratrol treatment in patients with polycystic ovary syndrome decreased pro-inflammatory and endoplasmic reticulum stress markers. Am J Reprod Immunol, 2020. 83(1): p. e13186.
103Chen, M., et al., Resveratrol ameliorates polycystic ovary syndrome via transzonal projections within oocyte-granulosa cell communication. Theranostics, 2022. 12(2): p. 782-795.
104Ortega, I. and A.J. Duleba, Ovarian actions of resveratrol. Ann N Y Acad Sci, 2015. 1348(1): p. 86-96.
105Mansour, A., et al., Effect of resveratrol on menstrual cyclicity, hyperandrogenism and metabolic profile in women with PCOS. Clin Nutr, 2021. 40(6): p. 4106-4112.
106Iervolino, M., et al., Natural Molecules in the Management of Polycystic Ovary Syndrome (PCOS): An Analytical Review. Nutrients, 2021. 13(5).
107Heshmati, J., et al., The effect of cinnamon supplementation on glycemic control in women with polycystic ovary syndrome: A systematic review and meta-analysis. J Food Biochem, 2021. 45(1): p. e13543.
108Heydarpour, F., et al., Effects of cinnamon on controlling metabolic parameters of polycystic ovary syndrome: A systematic review and meta-analysis. J Ethnopharmacol, 2020. 254: p. 112741.
109Maleki, V., et al., Mechanistic and therapeutic insight into the effects of cinnamon in polycystic ovary syndrome: a systematic review. J Ovarian Res, 2021. 14(1): p. 130.
110Tremellen, K. and K. Pearce, Dysbiosis of Gut Microbiota (DOGMA)–a novel theory for the development of Polycystic Ovarian Syndrome. Med Hypotheses, 2012. 79(1): p. 104-12.
111Yurtdaş, G. and Y. Akdevelioğlu, A New Approach to Polycystic Ovary Syndrome: The Gut Microbiota. J Am Coll Nutr, 2020. 39(4): p. 371-382.
112He, F.F. and Y.M. Li, Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. J Ovarian Res, 2020. 13(1): p. 73.
113Shamasbi, S.G., S. Ghanbari-Homayi, and M. Mirghafourvand, The effect of probiotics, prebiotics, and synbiotics on hormonal and inflammatory indices in women with polycystic ovary syndrome: a systematic review and meta-analysis. Eur J Nutr, 2020. 59(2): p. 433-450.
114Tabrizi, R., et al., The Effects of Probiotic Supplementation on Clinical Symptom, Weight Loss, Glycemic Control, Lipid and Hormonal Profiles, Biomarkers of Inflammation, and Oxidative Stress in Women with Polycystic Ovary Syndrome: a Systematic Review and Meta-analysis of Randomized Controlled Trials. Probiotics Antimicrob Proteins, 2022. 14(1): p. 1-14.
115Xu, Y., et al., Pretreatment with coenzyme Q10 improves ovarian response and embryo quality in low-prognosis young women with decreased ovarian reserve: a randomized controlled trial. Reprod Biol Endocrinol, 2018. 16(1): p. 29.
116Goodarzi, A., et al., The potential of probiotics for treating acne vulgaris: A review of literature on acne and microbiota. Dermatol Ther, 2020. 33(3): p. e13279.
As a Nutritionist, I’m continuing my mission to help women like you, beat PCOS. Evidence-based diet and lifestyle interventions helped me overcome five years of infertility. I fell pregnant naturally after multiple failed IVF cycles. Along the way, my other PCOS symptoms went away too. This experience taught me how to combine the latest science with a pragmatic approach to habit change. I’ve now helped thousands of other women achieve life-changing results, and I love for you to be the next PCOS success story. Learn more about me and what I do here.